An Rx for IT

Many of you know that, since this past summer, I have been working in a consulting role with a medical software company in Westborough, MA called eClinicalworks. I have learned a great deal about the role of technology in the delivery of healthcare.
Having 5 months of experience in the industry now certainly qualifies me to tell you exactly what is wrong with it and where the industry needs to go from here. Right?
Logic has always dictated that the most important reason to use computers is to lower costs and increase efficiency. A new study by the RAND Corporation shows this is simply not true. From the NYTimes yesterday:
“The conversion to electronic health records has failed so far to produce the hoped-for savings in health care costs and has had mixed results, at best, in improving efficiency and patient care, according to a new analysis by the influential RAND Corporation.”
Actually, the most important reason to use electronic medical records is to improve the health of our patients, to guard against errors, and to improve the overall experience for patients. Like Facebook, technologies can (in an ideal world) help us, as doctors, better communicate with our patients and to access their medical history (their “Timeline” as it were), and make the experience better and more streamlined for doctors and patients alike.
But, up to now, medical software hasn’t been designed to engage patients, it has been designed to improve physician billing. More attention has been paid to maximizing communication with payers and to making it easier to document an encounter to support the complexity needed for higher billing codes. Most EMRs will flawlessly communicate a charge electronically to any one of hundreds of health insurance companies, but still are unable to import your medical history and put the data in the right place in your chart!
People typically spend less than one hour a year with their doctors (and 8,759 hours per year checking their Facebook newsfeed and looking for cute pics of kittens on the Internet). Some people even skip that one-hour of visits all together. Combine this with studies that have shown that patients forget around 85% of what a doctor says during visits, ant that means, at best, my patients remember about nine minutes of everything I say per year.
What if that information had a chance to sink in? What would that do for our country’s health? What if instructions and education made it past the checkout window? What if we could remind our patients to take their pills or exercise? Send contextual health information in between visits? Prompt for important preventive procedures and tests? Of course, there’s all kinds of technology that exists to help us communicate with one another, e.g., Facebook, Skype, or text messaging. But you see very little of that designed to safely and securely facilitate communication between doctors and patients. That’s what our industry needs to be working on, tools to safely and securely mimic these types of technologies to improve the communication. (Part of the problem is, of course, health insurance doesn’t reimburse for such disruptive technologies and there is, therefore, less incentive for doctors to try, and little incentive for IT companies to work on this.)
Yet, this is what I am working on with eClinicalworks, new software to try and maximize the experience, and to make such communication easy and efficient for the doctors, and more accessible for the patients. I find it to be very rewarding work and I cannot wait to start using the fruits of our labor!
What about Nantucket? Could technology help to improve the healthcare delivery on Nantucket?
I think the answer is Yes and No or, better yet, “ought to” and “it ain’t going to happen!”
Right now, Nantucket is just another good example of the disease that is affecting Health IT nationally, the inability to exchange data between different systems. It is such a shame that this industry is so far behind other industries, such as the financial or shipping sectors. When I use my Stop & Shop card to purchase a box of Kraft Mac & Cheese, Kraft knows this, somehow, and automatically sends $0.03 as a refund to an organization called UPromise, which then deposits it into a 529 College Savings Fund I have with Fidelity (because I registered my S&S card with UPromise) and it shows up in my monthly emailed statement. And yet, if Dr. Lepore is out of town one day, and Dr. Butterworth sees one of his patients for an emergency, he is unable to see the record of that patient’s medicine allergies. This is unforgiveable (of our industry).
Nantucket’s health technology woes, like the nation’s as a whole, and are due to having multiple systems in place that do not talk to each other, causing a continued reliance on paper, making errors and oversights more likely to happen, and leading to inefficiencies in workflow.
The MGPO practices currently uses a record system called the LMR, which was written years ago for the physician practices at Mass General. Recognizing it’s difficulties in scaling to cover MGH’s expansion into new areas and hospital systems, as well as the trouble it has in integrating with other systems in place in their system as a whole, such as, the different systems for billing, and scheduling, and lab information, Mass General has recently signed a contract with Epic Systems to replace it with their software, and will spend over $600 million and 10 years to implement it! (And you wonder why your knee MRI is $3,000.)
My first concern about this is that if it is going to take 10 years to implement this, it’s hard for me to imagine the remote practices and smaller hospitals in the Partner’s system will be high on the list of priorities for installation. This will take a while.
My second concern is that Epic is a closed, legacy system. Using it, data communication (i.e., patient information) within Partner’s institutions should be improved. One database. One record. But Epic, as a closed system, is a shut door for this same data when it comes to communicating with other systems, e.g., smaller hospital systems, other ambulatory practices, radiology and lab centers, and even other systems using Epic.
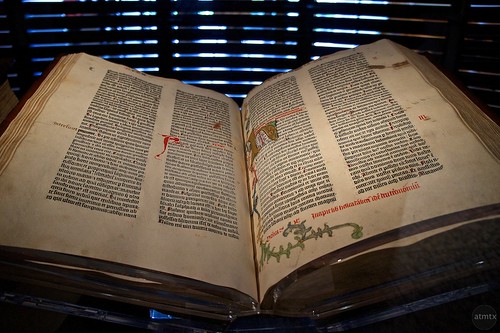
Finally, if it takes 10 years for them to implement it, I question whether or not this system will still be relevant. Ironically, even though it is a private company worth billions, Epic’s software is based on a computer language called MUMPS, the Massachusetts General Hospital Utility Multi-programming System, which was written 44 years ago, by scientists in an animal lab at Mass General! Forty-four years in computer programming years is akin to this haven been written as an addendum to the Gutenberg Bible! Since it is extremely challenging and costly for any organization that is not using it to interface with it, and since one of the biggest pushes in federal health regulation is towards the interchange of data, I question how relevant this software will be in 10 years. Certainly, if your goal was speed and efficiency, free and easy interchange of information, there are more modern “Cloud” technologies out there to be taken advantage of. But the problem is scaling these newer technologies to work in large hospital systems like Partners, and Johns Hopkins, and the Cleveland Clinic. And this is the niche Epic has created for themselves. This tried and true, if outdated, software makes it easier to customize large installations.
There was an interesting article in Forbes this past summer that discussed whether or not the hold Epic is developing on some of our larger hospital systems is a good thing or a bad thing for healthcare in general. My opinion is that closed systems are bad for healthcare as a whole.
In an ideal world, Nantucket’s hospital and handful of physician practices would have a unified software system in place that would allow for ease of use at the point of care, for patient online access to their records, secure messaging and improved communication with providers in between visits, and a safe but reliable and electronic exchange of information from the ER to the hospital to the lab to the doctor’s offices and to the patient. This system would also need to be open to communication from America, as it were, sending and receiving data from non-Partner’s and Partners hospitals (e.g., South Shore, Cape Cod, BIDMC, Dana Farber, Quest Labs, as well as MGH) and physicians.
Unfortunately, when it comes to Health Information Technology, there is no “ideal” world! Such a system does not exist. But as a small, contained health system, it would seem to me that if it were to be possible anywhere, it should be possible here! In the meantime, no good answers except to wait and see how long Epic takes to wash ashore.


January 12th, 2013 at 8:59 am
Greg, your never-ending thought processes astound me. You present such a dilemma for all of health care, not just MGH. Well if anyone can help with a solution, it’s you!
January 12th, 2013 at 11:22 am
Spot on, I deeply wish you success with implementation which will be revolutionary.
January 12th, 2013 at 7:06 pm
Wow! thanks for all that info! Maybe unrelated but I have a question… my next homebirth client (from MV) spent the entire fall in NYC being she is working on her Phd and has consistently asked her NY caregivers for print outs of her medical records (labs and prenatal care to date) and it is a nightmare! To then finally find out she can get them – and pick them up on the other side of Manhattan from the clinic and must pay $21 for them! Is this crazy? Never heard of such a thing, have you?
January 12th, 2013 at 7:27 pm
Nope. I think that is criminal. It’s her records!